In Short, Arnold Nerve Syndrome refers to a condition known as occipital neuralgia that leads to severe headaches in the occipital region of the head. This syndrome is characterized by intense, piercing pain that often radiates from the upper neck to the back of the skull. The primary benefits of understanding this condition include gaining insights into effective treatment options and coping strategies for those affected. Treatment typically involves pain management techniques, including medication and physical therapy, aimed at alleviating symptoms and improving quality of life. By addressing the underlying nerve irritation, individuals can experience significant relief from the debilitating effects of this painful condition. |
Arnold’s neuralgia, often referred to as occipital neuralgia, is a condition that leads to intense and debilitating headaches in the occipital region of the head. This disorder arises from irritation or injury to the occipital nerves, which can cause sharp, electric-shock-like pain radiating from the neck to the back and sides of the head. Patients often describe the sensation as piercing or throbbing, mimicking other ailments such as neck pain or torticollis. When it comes to addressing this condition, treatment options can range from medication management to therapeutic interventions aimed at alleviating discomfort and restoring quality of life. Understanding the symptoms and effective treatments is crucial for those affected by this painful syndrome.

Welcome to Pulse Align: Your Path to Natural Balance
Pulse Align is an innovative and non-invasive method designed to help restore your body’s natural posture and balance through gentle, imperceptible pulses. Clients often find this technique aids in reducing muscle and joint tension, leading to an enhanced sense of well-being.
Promoting Natural Recalibration
Rather than focusing on discomfort or specific conditions, Pulse Align facilitates the body’s inherent ability to recalibrate itself. This process often results in improved comfort and postural alignment, enabling clients to enjoy a more harmonious experience in their daily lives.
Personalized Approach to Wellness
At Pulse Align, we pride ourselves on our personalized approach. Clients frequently express their satisfaction with the noticeable improvements they experience in muscle tension and overall wellness, fostering a greater sense of balance and harmony. Discover firsthand how our gentle method has positively impacted individuals across various age groups and lifestyles.
Explore Pulse Align Today
We invite you to explore the benefits of Pulse Align for your entire family, including children and expectant mothers. Visit our website to learn more about how muscle tone symmetry can influence your overall well-being and find a clinic near you, whether it’s in La Prairie, Mont-Royal, Terrebonne, or other locations. Booking a consultation is simple and encourages you to experience our safe, non-invasive services that complement, but do not replace, medical care. Remember, any relief reported is attributed to your body’s natural ability to restore balance, not direct intervention from Pulse Align.
- Symptoms
- Piercing pain in the back of the head
- Sharp, jabbing electric shock sensations
- Throbbing discomfort behind the ears
- Tingling sensations along the scalp
- Piercing pain in the back of the head
- Sharp, jabbing electric shock sensations
- Throbbing discomfort behind the ears
- Tingling sensations along the scalp
- Treatments
- Physical therapy for pain relief
- Medications to reduce inflammation
- Botox injections for chronic headaches
- Occipital nerve blocks for immediate relief
- Physical therapy for pain relief
- Medications to reduce inflammation
- Botox injections for chronic headaches
- Occipital nerve blocks for immediate relief
- Piercing pain in the back of the head
- Sharp, jabbing electric shock sensations
- Throbbing discomfort behind the ears
- Tingling sensations along the scalp
- Physical therapy for pain relief
- Medications to reduce inflammation
- Botox injections for chronic headaches
- Occipital nerve blocks for immediate relief

Arnold Nerve Syndrome, also known as occipital neuralgia, is a condition characterized by intense, sharp headaches due to irritation or damage to the occipital nerves at the back of the head. The pain is often misinterpreted as other types of headaches, which complicates diagnosis and treatment. Understanding the symptoms, causes, and treatment options for this syndrome is crucial in managing your well-being effectively.
Symptoms of Arnold Nerve Syndrome
The hallmark of Arnold Nerve Syndrome is the severe, piercing pain that typically starts at the base of the skull and radiates through the back of the head and neck. Patients often describe the pain as a sharp, electric shock or a throbbing sensation. Other common symptoms include:
- Pain location: The discomfort often originates in the upper neck, especially around the occipital area, and can extend to the scalp.
- Trigger points: Even slight pressure on the affected area can provoke a sudden pain flare-up.
- Accompanying sensations: Patients may experience tingling, burning, or numbness that can further exacerbate the experience of pain.
Causes of Arnold Nerve Syndrome
The underlying factors leading to Arnold Nerve Syndrome generally stem from irritation or injury to the occipital nerves. Potential causes include:
- Trauma: Injury from accidents or medical procedures can significantly impact the occipital nerves.
- Muscle tension: Chronic contraction of neck muscles can lead to nerve compression, resulting in pain.
- Infections: Viral infections can trigger inflammation that impacts nerve function.
- Disease: Conditions like fibromyalgia or multiple sclerosis may also play a role in developing neuralgia.
Treatment Options for Arnold Nerve Syndrome
Addressing the symptoms of Arnold Nerve Syndrome requires a comprehensive approach tailored to individual needs. Effective treatment options include:
Medication management
Doctors may prescribe a combination of over-the-counter medication such as non-steroidal anti-inflammatory drugs (NSAIDs) and prescription medications like muscle relaxants or anticonvulsants to help alleviate pain. Nerve blocks using anesthetics may provide temporary relief for severe symptoms.
Physical therapy
Engaging in targeted physical therapy can assist in improving muscle function, enhancing mobility, and relieving pressure on the occipital nerves. Specific exercises designed to stretch and strengthen the neck and shoulder muscles can be effective in managing symptoms.
Alternative therapies
Incorporating alternative therapies such as acupuncture or chiropractic care may also offer relief, tapping into the body’s natural healing processes and addressing underlying imbalances.
Lifestyle changes
Implementing simple lifestyle modifications like practicing good posture, staying hydrated, and managing stress through mindfulness techniques can contribute significantly to minimizing flare-ups and enhancing overall quality of life.
| Aspect | Details |
| Symptoms | Piercing, throbbing pain in the back of the head. |
| Pain Type | Electric-shock-like sensations. |
| Location of Pain | Back of the head, neck, and behind the ears. |
| Triggers | Irritation or injury to the occipital nerves. |
| Initial Treatments | Heat application and rest. |
| Medications | Anti-inflammatory drugs and pain relievers. |
| Long-term Management | Physical therapy and nerve blocks. |
| Alternative Therapies | Acupuncture and relaxation techniques. |

Transformative Wellness Journey with Pulse Align
Clients experiencing Arnold Nerve Syndrome have shared transformative stories of holistic recovery thanks to Pulse Align’s dedicated approach to wellness. Many have discovered that their bodies have the innate ability to recalibrate and restore balance with the right support. The unique methodologies employed at Pulse Align have resonated well with individuals seeking relief from the debilitating symptoms associated with this condition.
For instance, individuals from La Prairie have expressed deep appreciation for how Pulse Align’s services align with their wellness goals. They reported feeling significant improvements in their daily lives as they engaged in treatments that not only addressed their pain but also empowered them to reclaim their health holistically. The support offered at Pulse Align goes beyond mere symptom relief; it connects clients to their bodies and fosters inner harmony.
Similar stories emerge from clients in Mont-Royal and Charlesbourg, who have embraced a holistic lifestyle while utilizing pulse alignment techniques. These clients have highlighted that their headaches have diminished in intensity, allowing them to engage more fully in family activities and social gatherings. Such improvements reflect the body’s capacity for natural healing when provided with the right environment and support.
In Sainte-Marie and Chicoutimi, individuals grappling with the effects of this syndrome have sought out Pulse Align’s services, motivated by a desire to enhance their overall well-being. Testimonials frequently emphasize how compassionate care and tailored treatments have made a measurable difference. Clients appreciate the collaborative effort between Pulse Align and their healthcare teams, which reassures them that they are not alone on this journey.
As clients report greater levels of comfort and functionality, it becomes clear that staying connected to Pulse Align can be beneficial. The lifelong wellness journey does not end with treatment; it often continues with ongoing care and community engagement. Clients from Deux-Montagnes have reaffirmed this sentiment, noting how they have not only gained insights and practical coping strategies, but also a supportive network of individuals who genuinely understand their experiences.
To explore these benefits further, clients in Panama City may find that coming together at Pulse Align fosters a reliable foundation for recovery and growth. When each individual’s journey is shared and honored, it creates an environment ripe for healing and empowerment.
For those seeking to experience this rejuvenating journey firsthand, we invite you to learn more about the supportive services provided by Pulse Align. Our commitment to work alongside healthcare teams to ensure comprehensive wellness reinforces our dedication to every client’s experience.
Discover our services at Our Clinics and witness how we can support your healing journey through a holistic lens.
Arnold Nerve Syndrome, also referred to as occipital neuralgia, involves pain stemming from the irritation or injury of the occipital nerves, which are located at the back of the head. This condition can lead to severe discomfort that often mimics other ailments, making diagnosis challenging. It typically presents with symptoms such as sharp, piercing pain that may radiate from the upper neck to the scalp, often described as feeling like an electric shock. Such acute sensations can be debilitating, impacting a person’s daily life and overall well-being.
The symptoms associated with Arnold Nerve Syndrome can vary in intensity and frequency. Patients may experience a throbbing headache that is localized to the occipital region. The discomfort is sometimes accompanied by tenderness, sensitivity, or even numbness in the neck and scalp. Individuals may also report episodes of pain that can be triggered by specific movements or pressure, further complicating their quality of life.
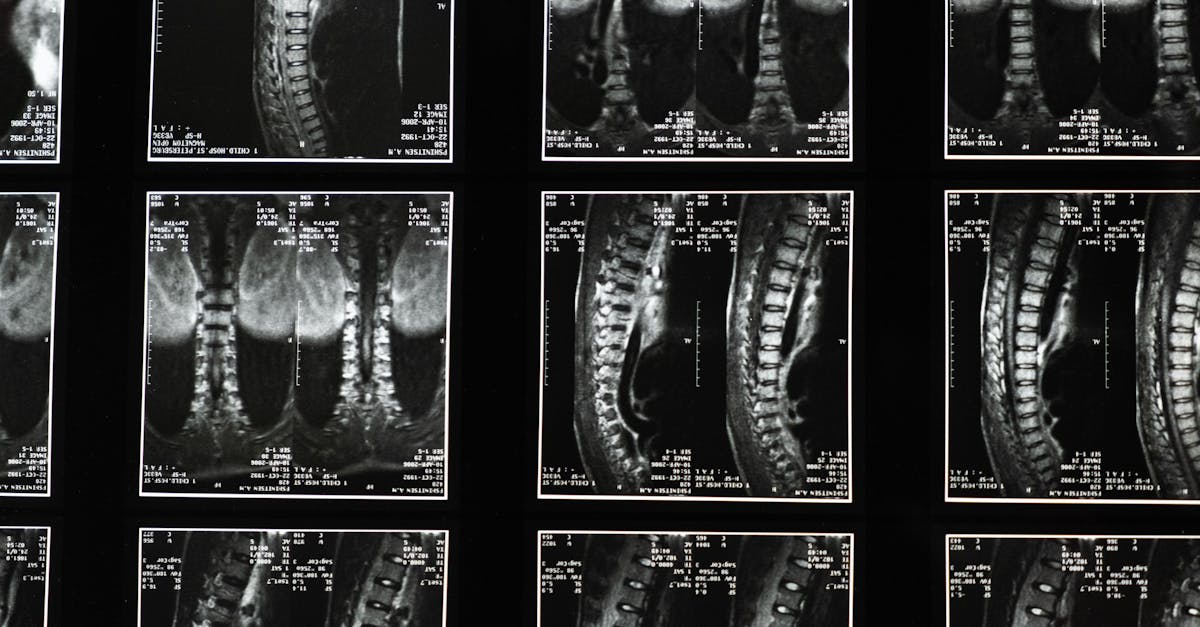
Diagnosis of Arnold Nerve Syndrome often requires a thorough assessment by healthcare professionals, particularly specialists in pain management or neurology. Given the overlapping symptoms with conditions such as tension-type headaches or migraines, a detailed medical history and physical examination are crucial. Advanced imaging techniques, like MRI or CT scans, may be utilized to rule out other potential causes of headache symptoms.
Treatment approaches for Arnold Nerve Syndrome are multifaceted and depend on the underlying causes, severity, and patient preferences. A multidisciplinary approach often yields the best outcomes. Neurologists or pain management specialists may recommend a combination of medications such as anti-inflammatory drugs, muscle relaxants, or even nerve blocks to alleviate discomfort. These interventions aim to reduce inflammation and provide temporary relief from pain.
In addition to pharmacological treatments, more innovative techniques are emerging in the management of Arnold Nerve Syndrome. Dr. Sylvain Desforges, an expert in osteopathy, naturopathy, and manual medicine, emphasizes the importance of integrating advanced technologies into patient care. His significant experience in chronic pain management includes the use of spinal decompression, laser therapy, and shockwave therapy at TAGMED clinics in Montreal. Each approach is tailored to enhance the healing process and optimize the health of his patients.
Furthermore, lifestyle modifications play a pivotal role in managing Arnold Nerve Syndrome. Patients are often encouraged to adopt gentle exercises, stretching routines, and relaxation techniques such as yoga or meditation, which can help reduce muscle tension and improve overall well-being. Ergonomic adjustments and proper posture can also alleviate stress on the neck and back, contributing to a decline in headache frequency.
Ultimately, the journey toward understanding and managing Arnold Nerve Syndrome involves both medical intervention and self-care strategies. Continuous communication with healthcare providers and exploring various treatment modalities are essential components in the quest for relief. As research expands and awareness grows, the hope is to enhance the quality of life for those affected by this painful condition.
Mechanism of Action
The neurovertebral decompression technology offered by TAGMED operates through a carefully controlled and progressive traction force applied to the spine. This innovative approach enhances the intervertebral space, effectively alleviating pressure on intervertebral discs and nerve roots. By facilitating an increase in the space between vertebrae, this technology promotes better fluid circulation in the targeted area, which is vital for reducing inflammation and providing pain relief. The strategic reduction in pressure can lead to a notable decrease in discomfort experienced by individuals struggling with conditions like disc herniation, bulging discs, and moderate to severe spinal stenosis.
Specific Benefits
This non-invasive method is designed to effectively alleviate chronic pain and symptoms associated with various spinal afflictions. The direct impact of this technology reduces the pressure exerted on nerve structures and optimizes fluid circulation around the discs, thereby promoting quicker recovery times and an enhanced quality of life for a diverse range of patients. Moreover, by addressing the underlying issues associated with spinal conditions, TAGMED’s approach helps patients avoid the complications often linked to more invasive procedures.
Comparison with Other Treatments
When juxtaposed with traditional treatments, such as analgesics, corticosteroid injections, surgery, or conventional physiotherapy, TAGMED’s neurovertebral decompression technology stands out due to its unique advantages. This method eliminates the risks typically associated with invasive interventions and reduces potential adverse effects from medication. Patients often experience faster recovery times, thus enabling a swift return to daily activities without the long-lasting consequences associated with surgical options.
Case Studies or Testimonials
Numerous patients have reported significant improvements following TAGMED’s neurovertebral decompression therapy for managing their chronic pain and associated symptoms. For instance, individuals have observed a sustainable decrease in pain levels, a quicker return to their regular routines, and a notable reduction in reliance on pharmacological treatments. These testimonials underscore the effectiveness of this approach and highlight its potential to transform the lives of those living with chronic pain conditions.
Neurovertebral decompression technology represents a significant advancement in the non-invasive treatment of chronic pain and spinal conditions. Its ability to relieve pressure on neural structures while optimizing the body’s natural healing processes positions it as a valuable alternative to traditional treatments.
The term Arnold’s Neuralgia, also referred to as occipital neuralgia, encapsulates a painful condition characterized by the irritation of the occipital nerves, which are responsible for sensation in the back of the head and neck. This condition is not merely an inconvenience but can be debilitating, causing those affected to experience severe, sharp, or throbbing headaches. These headaches typically commence from the upper neck and ascend to the back of the head, sometimes mimicking other disorders such as temporary neck pain or torticollis.
One of the most pressing issues surrounding Arnold’s Neuralgia is its presentation of symptoms. Individuals often describe their pain as piercing, electric shock-like, or a jabbing sensation that can leave them feeling incapacitated. These symptoms are particularly distressing due to their intensity and can lead to significant disruptions in daily activities, making accurate diagnosis and treatment crucial for effective management.
Treatment for Arnold’s Neuralgia can be varied and may include a combination of medications, physical therapy, and in some cases, surgical intervention. Medications such as anti-inflammatory drugs or anticonvulsants are often prescribed to alleviate the pain and reduce inflammation. Physical therapy may focus on alleviating tension in the neck and improving posture, which has been shown to provide relief for some patients. In more severe cases, nerve blocks or surgical procedures may be options considered by healthcare professionals.
Overall, understanding Arnold Nerve Syndrome is essential for those experiencing its symptoms. Increased awareness can foster better communication with healthcare providers and encourage patients to seek help sooner. This proactive approach could lead to appropriate treatment pathways and ultimately improve quality of life for individuals suffering from this challenging condition.

Do you suffer from a chronic condition that responds little or not at all to conservative treatments?
In today’s fast-paced world, many individuals seek holistic approaches to restore balance and improve overall well-being. Pulse Align offers a unique, non-invasive method designed to support the body’s natural recalibration process through gentle, imperceptible pulses. This innovative approach helps address muscle tension and joint discomfort, promoting an enhanced sense of comfort and posture, creating a pathway for clients to explore a natural way to feel better.
At Pulse Align, the focus is not on specific discomforts or conditions. Instead, the aim is to help the body recalibrate itself, enhancing muscle tone symmetry and promoting improved posture. Clients often report experiencing remarkable enhancements in their overall comfort and well-being as their bodies regain balance and strength from within. This gentle approach resists conventional methods and instead embraces the body’s inherent ability to thrive.
Pulse Align takes pride in its personalized approach to wellness. Numerous testimonials highlight the positive experiences of clients who have enjoyed remarkable improvements in neck and back tension, as well as an overall sense of wellness. Clients find a welcoming environment where their unique needs are acknowledged, allowing them to feel empowered on their wellness journey without the need for medical interventions.
We invite you to explore Pulse Align by visiting our website. Discover nearby locations in cities such as La Prairie, Mont-Royal, or Terrebonne, and book a consultation for yourself or your entire family. Remember, Pulse Align complements, but does not replace, any existing healthcare services. Our approach is family-friendly and suitable for all ages, reassuring clients that their wellness journey is in good hands.
With our cutting-edge, non-invasive technology, Pulse Align works to restore muscle tone symmetry, helping to alleviate tension in the spine and other areas gently. This service is safe for pregnant women and young children, ensuring that everyone in the family can benefit from our personalized, humane interventions. We encourage you to book an appointment online today and take the first step towards a well-balanced and thriving lifestyle.
Frequently Asked Questions
Headache and Migraine
- Can identifying triggers reduce migraines?Yes, keeping a headache diary helps identify triggers so you can avoid them.
- Does bright light trigger migraines?Yes, light sensitivity is common, and bright light can worsen a migraine attack.
- Are over-the-counter pain relievers effective?They can relieve occasional headaches, but frequent use may lead to rebound headaches.
- Is stress a trigger?Yes, physical or emotional stress is among the most common headache and migraine triggers.
- Is an aura always present?No, only about 20% of migraine sufferers experience an aura before the attack.
- Should I avoid physical exertion during a migraine?Intense activity may worsen the attack; rest in a quiet, dark room is often recommended.
- Can migraines occur at night?Yes, some people wake up with migraines, sometimes linked to sleep disorders.
- What’s the difference between a headache and a migraine?A headache is often less intense and short-lived, while a migraine is characterized by throbbing pain, sometimes with nausea, sensitivity to light and sound.
- How to differentiate a migraine from a tension headache?Tension headaches cause diffuse, moderate pressure. Migraines are often more severe, pulsating, one-sided, and accompanied by associated symptoms.
- Does noise trigger migraines?Yes, hypersensitivity to sound is common, and loud noises can worsen the pain.
Ethan Dubois is dedicated to shining a light on the hidden struggles of chronic headaches. As a Headache Awareness Advocate at Pulse Align, he combines compassionate storytelling with cutting-edge research to bring clarity, comfort, and hope to those affected. Ethan’s mission is to empower readers with knowledge, break through stigma, and foster a supportive community where every voice is heard. When he’s not crafting insightful articles, Ethan can be found exploring the latest wellness trends, sharing practical coping strategies, or simply lending a listening ear to those in need. His heartfelt approach and unwavering commitment to awareness make him a trusted ally for anyone navigating life with headaches.
References
- Bjarne, B. (2024). NECK MUSCLE ELASTICITY IN CERVICOGENIC HEADACHE PATIENTS MEASURED BY SHEAR WAVE ELASTOGRAPHY [PhD Thesis, Ghent University]. https://libstore.ugent.be/fulltxt/RUG01/003/202/979/RUG01-003202979_2024_0001_AC.pdf
- Lin, L.-Z., Yu, Y.-N., Fan, J.-C., Guo, P.-W., Xia, C.-F., Geng, X., Zhang, S.-Y., & Yuan, X.-Z. (2022). Increased stiffness of the superficial cervical extensor muscles in patients with cervicogenic headache: A study using shear wave elastography. Frontiers in Neurology, 13, 874643. https://www.frontiersin.org/articles/10.3389/fneur.2022.874643/full
- Pradhan, S., & Choudhury, S. S. (2018). Clinical characterization of neck pain in migraine. Neurology India, 66(2), 377–384. https://journals.lww.com/neur/fulltext/2018/66020/clinical_characterization_of_neck_pain_in_migraine.19.aspx
- Balaban, M., Celenay, S. T., Lalecan, N., Akan, S., & Kaya, D. O. (2024). Morphological and mechanical properties of cervical muscles in fibromyalgia with migraine: A case-control study. Musculoskeletal Science and Practice, 74, 103185. https://www.sciencedirect.com/science/article/pii/S2468781224002807
- Martínez-Merinero, P., Aneiros Tarancón, F., Montañez-Aguilera, J., Nuñez-Nagy, S., Pecos-Martín, D., Fernández-Matías, R., Achalandabaso-Ochoa, A., Fernández-Carnero, S., & Gallego-Izquierdo, T. (2021). Interaction between pain, disability, mechanosensitivity and cranio-cervical angle in subjects with cervicogenic headache: A cross-sectional study. Journal of Clinical Medicine, 10(1), 159. https://www.mdpi.com/2077-0383/10/1/159
- Al-Khazali, H. M., Al-Sayegh, Z., Younis, S., Christensen, R. H., Ashina, M., Schytz, H. W., & Ashina, S. (2024). Systematic review and meta-analysis of Neck Disability Index and Numeric Pain Rating Scale in patients with migraine and tension-type headache. Cephalalgia, 44(8), 03331024241274266. https://doi.org/10.1177/03331024241274266
- Zwart, J. (1997). Neck Mobility in Different Headache Disorders. Headache: The Journal of Head and Face Pain, 37(1), 6–11. https://doi.org/10.1046/j.1526-4610.1997.3701006.x
- Choi, S.-Y., & Choi, J.-H. (2016). The effects of cervical traction, cranial rhythmic impulse, and Mckenzie exercise on headache and cervical muscle stiffness in episodic tension-type headache patients. Journal of Physical Therapy Science, 28(3), 837–843. https://www.jstage.jst.go.jp/article/jpts/28/3/28_jpts-2015-893/_article/-char/ja/
- Aoyama, N. (2021). Involvement of cervical disability in migraine: a literature review. British Journal of Pain, 15(2), 199–212. https://doi.org/10.1177/2049463720924704
- Hvedstrup, J., Kolding, L. T., Ashina, M., & Schytz, H. W. (2020). Increased neck muscle stiffness in migraine patients with ictal neck pain: A shear wave elastography study. Cephalalgia, 40(6), 565–574. https://doi.org/10.1177/0333102420919998
- Fernández-de-las-Peñas, C., Cuadrado, M., & Pareja, J. (2006). Myofascial Trigger Points, Neck Mobility and Forward Head Posture in Unilateral Migraine. Cephalalgia, 26(9), 1061–1070. https://doi.org/10.1111/j.1468-2982.2006.01162.x
- Luedtke, K., Starke, W., & May, A. (2018). Musculoskeletal dysfunction in migraine patients. Cephalalgia, 38(5), 865–875. https://doi.org/10.1177/0333102417716934
- Fernández-de-las-Peñas, C., Madeleine, P., Caminero, A., Cuadrado, M., Arendt-Nielsen, L., & Pareja, J. (2010). Generalized Neck-Shoulder Hyperalgesia in Chronic Tension-Type Headache and Unilateral Migraine Assessed by Pressure Pain Sensitivity Topographical Maps of the Trapezius Muscle. Cephalalgia, 30(1), 77–86. https://doi.org/10.1111/j.1468-2982.2009.01901.x
- Fernández‐de‐las‐Peñas, C., Cuadrado, M. L., & Pareja, J. A. (2007). Myofascial Trigger Points, Neck Mobility, and Forward Head Posture in Episodic Tension‐Type Headache. Headache: The Journal of Head and Face Pain, 47(5), 662–672. https://doi.org/10.1111/j.1526-4610.2006.00632.x
- Kolding, L. T., Do, T. P., Ewertsen, C., & Schytz, H. W. (2018). Muscle stiffness in tension-type headache patients with pericranial tenderness: A shear wave elastography study. Cephalalgia Reports, 1, 2515816318760293. https://doi.org/10.1177/2515816318760293
- Ashina, S., Bendtsen, L., Lyngberg, A. C., Lipton, R. B., Hajiyeva, N., & Jensen, R. (2015). Prevalence of neck pain in migraine and tension-type headache: A population study. Cephalalgia, 35(3), 211–219. https://doi.org/10.1177/0333102414535110
- Florencio, L. L., De Oliveira, A. S., Carvalho, G. F., Tolentino, G. D. A., Dach, F., Bigal, M. E., Fernández‐de‐las‐Peñas, C., & Bevilaqua Grossi, D. (2015). Cervical Muscle Strength and Muscle Coactivation During Isometric Contractions in Patients With Migraine: A Cross‐Sectional Study. Headache: The Journal of Head and Face Pain, 55(10), 1312–1322. https://doi.org/10.1111/head.12644
- Al-Khazali, H. M., Younis, S., Al-Sayegh, Z., Ashina, S., Ashina, M., & Schytz, H. W. (2022). Prevalence of neck pain in migraine: A systematic review and meta-analysis. Cephalalgia, 42(7), 663–673. https://doi.org/10.1177/03331024211068073
- Yu, Z., Wang, R., Ao, R., & Yu, S. (2019). Neck pain in episodic migraine: a cross-sectional study. Journal of Pain Research, Volume 12, 1605–1613. https://doi.org/10.2147/JPR.S200606
- Calhoun, A. H., Ford, S., Millen, C., Finkel, A. G., Truong, Y., & Nie, Y. (2010). The Prevalence of Neck Pain in Migraine. Headache: The Journal of Head and Face Pain, 50(8), 1273–1277. https://doi.org/10.1111/j.1526-4610.2009.01608.x